What’s Really Going On When High Blood Pressure Causes Headaches
Discover What’s Really Going On When High Blood Pressure Causes Headaches. Learn the truth behind this common condition and its symptoms.
Sarah rubbed her temples as another pounding headache set in. She’d recently been diagnosed with hypertension, but her doctor never mentioned headaches as a common issue. After checking her monitor, she stared at the elevated numbers—could there be a connection?
Medical experts have debated this question for decades. While some studies suggest a link between blood pressure spikes and head pain, others find no clear pattern. The American Heart Association notes most people won’t feel symptoms unless readings soar above 180/120 mm Hg—a critical threshold requiring immediate care.
Why the confusion? Research methods vary widely, from patient self-reports to clinical measurements. A 2021 review highlighted how these differences create conflicting conclusions. Many with mild hypertension never experience head discomfort, while those with severe cases might—but it’s rarely the sole warning sign.
This uncertainty leaves patients like Sarah wondering: Is it stress, dehydration, or something more serious? We’ll unravel the science behind these overlapping conditions and explain when elevated numbers truly demand attention.
Key Takeaways
- Most individuals with mild/moderate hypertension don’t experience headaches directly from elevated blood pressure
- Headaches typically occur only during hypertensive crises (readings above 180/120 mm Hg)
- Research conflicts stem from differing study designs and measurement techniques
- Headaches and hypertension often coexist without direct causation
- Always consult a doctor for persistent head pain with high blood pressure readings
Understanding High Blood Pressure and Its Effects
Nearly half of U.S. adults carry a silent burden that strains their organs quietly. This condition, called hypertension, often develops without obvious warnings. Many don’t realize their numbers creep upward until a routine checkup reveals the truth.
Defining Hypertension and Its Silent Nature
Medical professionals label readings above 130/80 mmHg as elevated. Yet most with these numbers feel completely normal. “Patients often assume they’d notice something wrong,” says cardiologist Luke Laffin, MD. “But the body adapts until damage becomes severe.”
Undetected hypertension acts like slow-acting rust in pipes. It weakens artery walls while forcing the heart to pump harder. Over years, this strain can lead to kidney filtration issues and narrowed blood vessels.
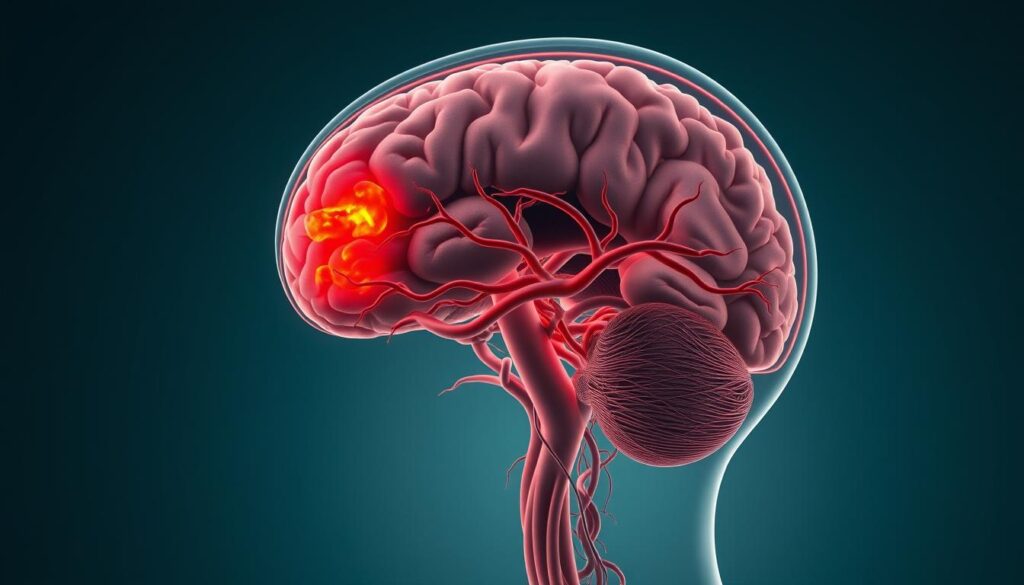
How Elevated Levels Impact Vital Organs
Consistently high pressure transforms blood flow into a destructive force. Your arteries stiffen, reducing oxygen delivery to tissues. The kidneys filter less efficiently, allowing waste buildup.
Meanwhile, delicate brain vessels face increased risk of leaks or blockages. These changes occur gradually, explaining why regular monitoring proves crucial for long-term health protection.
What’s Really Going On When High Blood Pressure Causes Headaches
Imagine your brain swelling against the unyielding walls of your skull—this hidden drama explains some hypertension-related head discomfort. Recent studies reveal how extreme elevations strain delicate biological systems, creating a perfect storm for pulsating pain.
Medical Insights and Research Findings
Neurologists have identified a critical threshold where blood pressure spikes overwhelm the brain’s protective mechanisms. “At dangerous levels, fluid breaches the blood-brain barrier like a dam cracking under pressure,” explains Dr. Anita Rao, a vascular specialist. This leakage triggers swelling that presses against rigid bone, intensifying discomfort during movement.
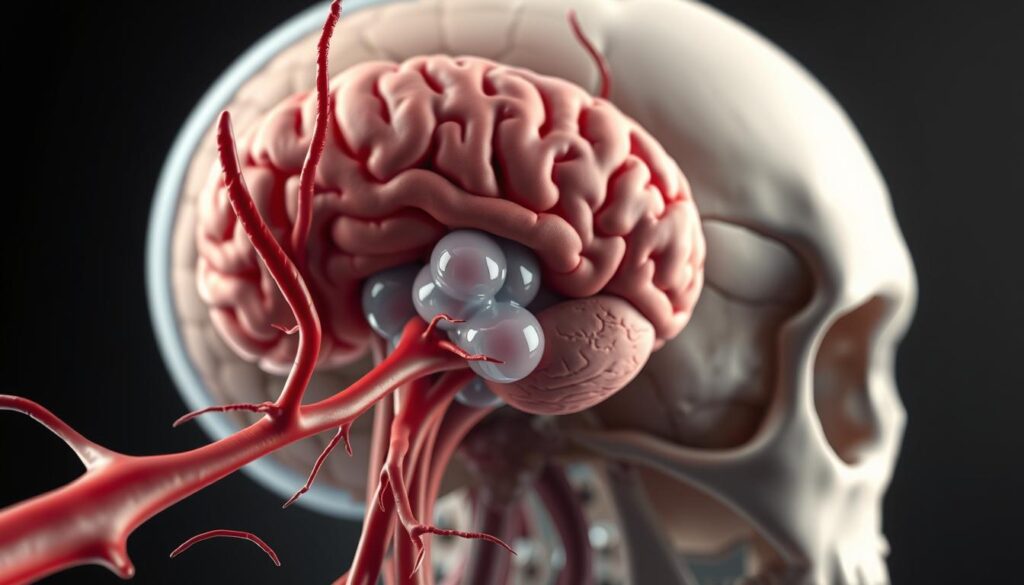
Perspectives on the Blood-Brain Barrier and Edema
Your brain’s security system—the blood-brain barrier—normally filters harmful substances. When hypertension forces excessive fluid through blood vessel walls, tissues swell like a sponge absorbing water. The resulting pressure often manifests as:
| Headache Type | Key Features | Worsening Factors |
|---|---|---|
| Tension | Band-like pressure | Stress |
| Migraine | One-sided throbbing | Light/sound |
| Hypertension-Related | Bilateral pulsating | Physical activity |
This table highlights why monitoring blood pressure during head pain matters. Unlike other types, hypertension-induced discomfort directly reflects physical changes in cranial structures. Always consult a healthcare provider if symptoms align with the third category.
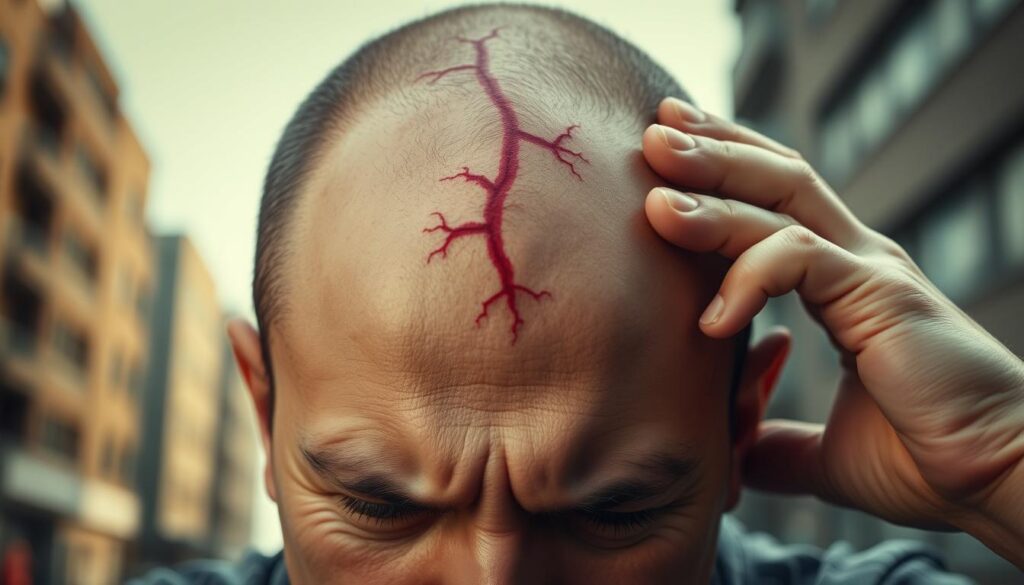
Exploring the Hypertensive Crisis and Headache Connection
A sudden, crushing headache strikes without warning—your body’s alarm system blaring at maximum volume. This intense pain often signals a hypertensive crisis, where readings leap past 180/120 mmHg. While some cases involve no immediate danger (hypertensive urgency), others become emergencies demanding swift action.
Recognizing the Signs of a Hypertensive Emergency
“Think of it as your cardiovascular system screaming for help,” explains ER physician Dr. Mark Torres. Distinct from routine headaches, this pain typically hits both sides of the head like a vise. Accompanying symptoms reveal multi-organ distress:
| Warning Sign | Body System Affected | Action Required |
|---|---|---|
| Chest pressure | Heart | Call 911 |
| Blurred vision | Eyes | Seek ER care |
| Nausea/vomiting | Digestive | Immediate evaluation |
Time becomes your greatest enemy during these events. A 2017 review found nearly 5% of patients in cardiac units don’t survive hypertensive emergencies. Those experiencing severe headache with any listed symptoms should seek medical attention within 60 minutes—every moment counts when organs face potential failure.
Lifestyle, Diet, and Medication: Managing the Dual Challenge
Balancing nutrition and prescriptions becomes a tightrope walk when managing two health concerns simultaneously. Smart choices in daily habits can ease both conditions while preventing conflicts between treatments.
Dietary Choices and Their Impact
Food triggers affect 20% of people with recurrent head pain. Common culprits include:
- Processed meats containing nitrates
- Artificial sweeteners in diet drinks
- Aged cheeses and fermented foods
Swapping omega-6-heavy oils for olive oil or walnuts may reduce inflammation. Dr. Elena Morris, a nutrition researcher, notes: “Small dietary shifts often yield dual benefits—better vessel health and fewer headache days.”
Safe Use of Medications
Over-the-counter pain relievers require caution with blood pressure medication. Aspirin works for most, but avoid NSAIDs like ibuprofen if taking diuretics. Always:
- Check labels for sodium content
- Space doses 4+ hours apart from prescriptions
- Report new symptoms to your doctor
Non-Drug Treatments
Proven stress-reduction methods include:
- Guided breathing exercises (4-7-8 technique)
- Evening yoga sessions
- Consistent sleep schedules
These approaches help regulate circulatory strain without risking medication interactions. Weekly mindfulness practice shows a 31% reduction in headache frequency according to recent trials.
Debunking Myths and Addressing Common Misconceptions
Many assume throbbing temples automatically signal dangerous blood pressure levels. Let’s separate fact from fiction using data from one of medicine’s longest-running studies.
Myths vs. Facts: The Reality Behind Co-Occurrence
A 30-year study tracking 1,914 participants with hypertension revealed surprising patterns. Researchers found no connection between frequent headaches and heart-related deaths. “This data challenges decades of assumptions,” notes cardiologist Dr. Emily Carter.
| Myth | Fact | Evidence |
|---|---|---|
| Morning headaches mean BP spikes | Dehydration/sleep issues cause most morning pain | Journal of Clinical Sleep Medicine (2019) |
| Headaches indicate poor BP control | 83% with controlled hypertension report headaches | American Heart Association data |
| Pain frequency predicts heart risk | No mortality difference in headache sufferers | AJH study findings |
Why the confusion? Both conditions affect 46% of U.S. adults. This overlap creates false connections. While blood pressure cause headaches in crises, daily discomfort usually stems from:
- Stress hormones
- Caffeine withdrawal
- Eye strain
Tracking symptoms helps identify true patterns. Those concerned should monitor readings during pain episodes rather than assume causation.
Conclusion
When severe head pain strikes with elevated readings, act fast—this combo often signals urgent health risks. While daily headaches rarely stem from mild blood pressure changes, sudden crushing pain paired with extreme numbers demands immediate care. “It’s like your body flashing red emergency lights,” explains nurse practitioner Laura Chen.
Track patterns carefully. Headaches might temporarily raise your numbers rather than result from them. Research shows stress-induced pain can spike readings by 20+ points temporarily. But sustained elevations during episodes could indicate hypertensive crisis risks.
Keep these action steps handy:
• Check readings during severe headaches
• Note accompanying symptoms like chest tightness
• Contact your doctor if numbers exceed 180/120 mmHg
Protect your long-term health through regular monitoring and open communication with care providers. Remember—consistent management beats guessing games when balancing head discomfort and circulatory concerns.