Understanding Gut Imbalance: Signs and Causes
Common Symptoms of an Unhealthy Gut
Your gut is trying to tell you something when it’s not functioning properly. The most obvious signs show up in your digestive system first. Bloating, excessive gas, and stomach discomfort aren’t just annoying – they’re your body’s alarm bells. That uncomfortable full feeling that doesn’t match what you’ve eaten, or the embarrassing gas that seems to come out of nowhere? These are primary indicators that your gut microbiome may be out of balance.
Pay attention to your bathroom habits too. Are you running to the bathroom multiple times a day with loose stools? Or maybe you’re struggling to go at all? Both diarrhea and constipation signal that something’s off with your digestive system. Healthy bowel movements should be relatively consistent in timing and texture—not too hard, not too soft.
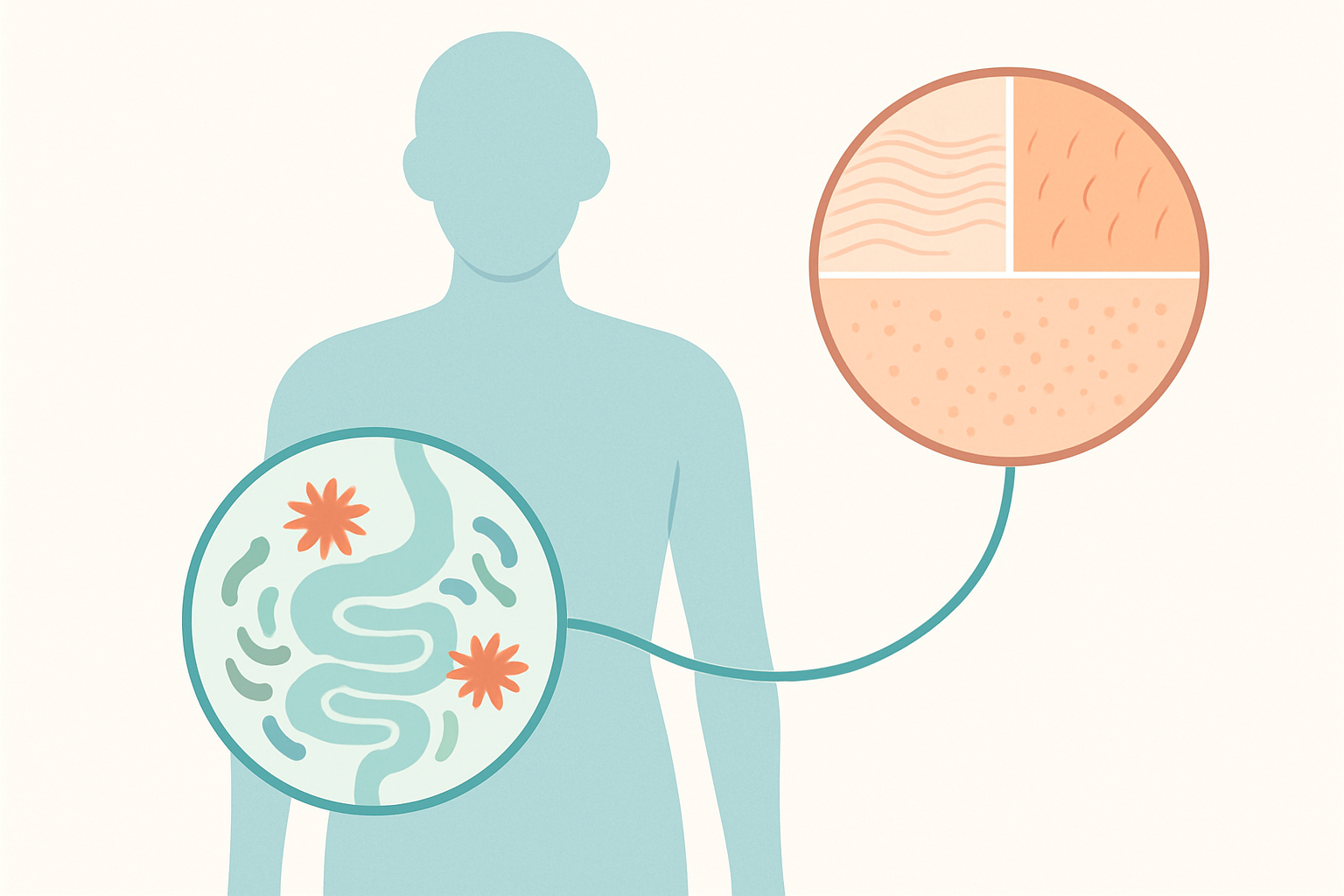
What surprises many people is how gut issues can affect areas seemingly unrelated to digestion. Persistent fatigue that doesn’t improve with sleep might actually stem from poor nutrient absorption in your gut. That foggy thinking that makes concentration difficult? Your gut bacteria produce neurotransmitters that affect brain function. Even skin problems like acne, eczema, or unexplained rashes often trace back to gut inflammation.
Over time, an imbalanced gut can lead to food sensitivities you never had before. Suddenly feeling bloated after eating dairy or getting headaches from gluten-containing foods might indicate your gut lining has become more permeable—sometimes called “leaky gut”—allowing food particles to trigger immune responses they normally wouldn’t.
Major Causes of Gut Disruption
The modern Western lifestyle is practically designed to disrupt gut health. Processed foods loaded with refined sugars, artificial additives, and unhealthy fats starve beneficial bacteria while feeding harmful ones. High-sugar diets particularly cause rapid microbiome shifts that promote inflammation and digestive distress.
Your stress levels dramatically impact your digestion too. When you’re anxious or chronically stressed, your body diverts energy away from proper digestion. Stress hormones like cortisol directly affect gut motility (how food moves through your system), enzyme production, and even the composition of your gut bacteria.
Antibiotics, while sometimes necessary, act like carpet bombs in your gut. They don’t just kill harmful bacteria causing infection—they wipe out beneficial ones too. Just one course of antibiotics can alter your gut microbiome for months or even years without proper restoration.
Your daily rhythms also matter tremendously. Irregular sleep patterns disrupt the circadian rhythms that guide your digestive processes. Similarly, erratic eating patterns—skipping meals, eating late at night, or constant snacking—never give your digestive system the rest periods it needs to function properly.
The Microbiome Connection
Your gut houses trillions of microorganisms—bacteria, viruses, fungi, and other microscopic creatures—collectively called your microbiome.
This bustling community isn’t just along for the ride; it actively participates in digestion, vitamin production, immune function, and even hormone regulation.
Diversity is the hallmark of a healthy microbiome. Different bacterial species perform different functions, from breaking down specific food components to producing essential fatty acids. When this diversity drops, certain digestive processes become inefficient or completely defunct.
The gut-brain connection is one of medicine’s most fascinating discoveries. Your gut and brain constantly communicate through the vagus nerve, hormones, and immune signals. This explains why digestive distress so often accompanies anxiety or depression. Your gut bacteria actually produce most of your body’s serotonin – a key mood-regulating neurotransmitter.
When your microbiome falls out of balance (dysbiosis), inflammation typically follows. This inflammatory response doesn’t just stay in your gut – it can become systemic, triggering pain, autoimmune responses, and chronic disease processes throughout your body.
Days 1-3: Elimination and Hydration Foundation
Day 1: Remove Gut Irritants
Your gut reset begins with removing the most common irritants that disrupt digestive harmony. Start by clearing your kitchen of processed foods containing artificial preservatives, colors, and flavors. These chemicals can irritate your gut lining and disturb your microbiome balance.
Cut out alcohol completely for this week—even that “one glass” of wine can trigger inflammation and disrupt beneficial bacteria. Similarly, scale back caffeine to one cup in the morning if you can’t eliminate it entirely, as excessive caffeine can stimulate acid production and irritate your digestive tract.
Pay close attention to how your body responds to common trigger foods. Dairy and gluten are frequent culprits for many people. Remove these from your diet temporarily, even if you don’t have a known intolerance. Other potential triggers include soy, eggs, corn, and nightshades (tomatoes, peppers, eggplant).
When grocery shopping, read labels carefully. Look for hidden gut disruptors like:

– Artificial sweeteners (aspartame, sucralose) – Carrageenan – High-fructose corn syrup – MSG (often disguised as “natural flavors” or “hydrolyzed protein”)
Focus meals around simple, whole foods. Try a breakfast of overnight oats with berries, lunch of leafy greens with roasted vegetables and wild-caught salmon, and dinner featuring baked sweet potato with steamed vegetables and grilled chicken. Keep snacks minimalist—think apple slices with almond butter or carrot sticks with hummus.
Day 2: Optimizing Hydration
Proper hydration is foundational for gut healing. Aim to drink at least half your body weight in ounces daily (e.g., 75 oz for a 150-pound person). This helps move waste through your digestive system and maintains the mucus lining that protects your gut wall.
Surprisingly, room temperature water supports digestion better than ice-cold water, which can shock your system and constrict digestive vessels. Start your morning with warm water before consuming anything else.
Enhance your hydration with gut-friendly additions:

– Lemon water (supports liver function and stimulates digestive enzymes) – Cucumber slices (contain anti-inflammatory compounds) – Sliced ginger (reduces intestinal inflammation and speeds digestion) – Fresh mint leaves (soothes digestive discomfort and reduces bloating)
Create a consistent hydration schedule by drinking a full glass of water when you wake up, 30 minutes before each meal, mid-morning, mid-afternoon, and an hour before bed. This prevents you from becoming dehydrated and helps establish regular bowel movements.
Day 3: Introducing Digestive Enzymes and Stomach Acid Support
By day three, focus on optimizing your body’s natural digestive processes. Start your morning with 1-2 tablespoons of raw apple cider vinegar in water before breakfast to stimulate stomach acid production. Low stomach acid is surprisingly common and can severely impair digestion.
Implement proper meal timing by waiting 3-4 hours between meals to allow full digestion. Practice mindful eating by chewing each bite 20-30 times. This seemingly simple practice dramatically improves digestion by reducing the workload on your stomach and small intestine while properly mixing food with saliva enzymes.
Before meals, try this 30-second digestive preparation ritual: Take three deep breaths and place one hand on your belly, signaling to your body that food is coming. This activates your parasympathetic nervous system—essential for proper digestion.
Incorporate bitter foods like arugula, dandelion greens, or endive into your meals. These naturally stimulate bile production, which helps break down fats and supports liver detoxification pathways crucial for gut health.
Days 4-6: Rebuilding Gut Flora and Reducing Inflammation
Day 4: Introducing Probiotic-Rich Foods
Now that you’ve removed irritants and improved your digestive foundation, it’s time to repopulate your gut with beneficial bacteria. Fermented foods are your best friends here!

Look for these easy-to-find probiotic powerhouses at your local grocery store:
- Plain unsweetened yogurt with live cultures
- Kombucha (low-sugar varieties)
- Sauerkraut (refrigerated, not canned)
- Kimchi
- Miso paste
- Tempeh
- Kefir (dairy or water-based)
Making your own fermented foods is simpler than you might think. Try this quick pickle recipe: thinly slice cucumbers, add to a jar with 1 cup water, 1 tablespoon sea salt, and 2 tablespoons apple cider vinegar. Leave at room temperature for 24-48 hours, then refrigerate.
For homemade kefir, mix kefir grains with milk and let sit for 24 hours at room temperature. Strain and enjoy!
Start with small servings – just 1-2 tablespoons of fermented vegetables or 4-6 ounces of yogurt or kefir daily. Too much too soon can cause gas and bloating. Gradually increase to 1/4 cup fermented vegetables or 1 cup of yogurt/kefir daily.
Certain food pairings boost probiotic benefits. Try yogurt with berries (the polyphenols act as food for probiotics) or sauerkraut on a turkey sandwich (protein helps probiotic survival through stomach acid).
Day 5: Focus on Prebiotic Fiber
While probiotics are beneficial bacteria, prebiotics are the food that helps these good bacteria thrive. Think of probiotics as the seeds and prebiotics as the fertilizer.
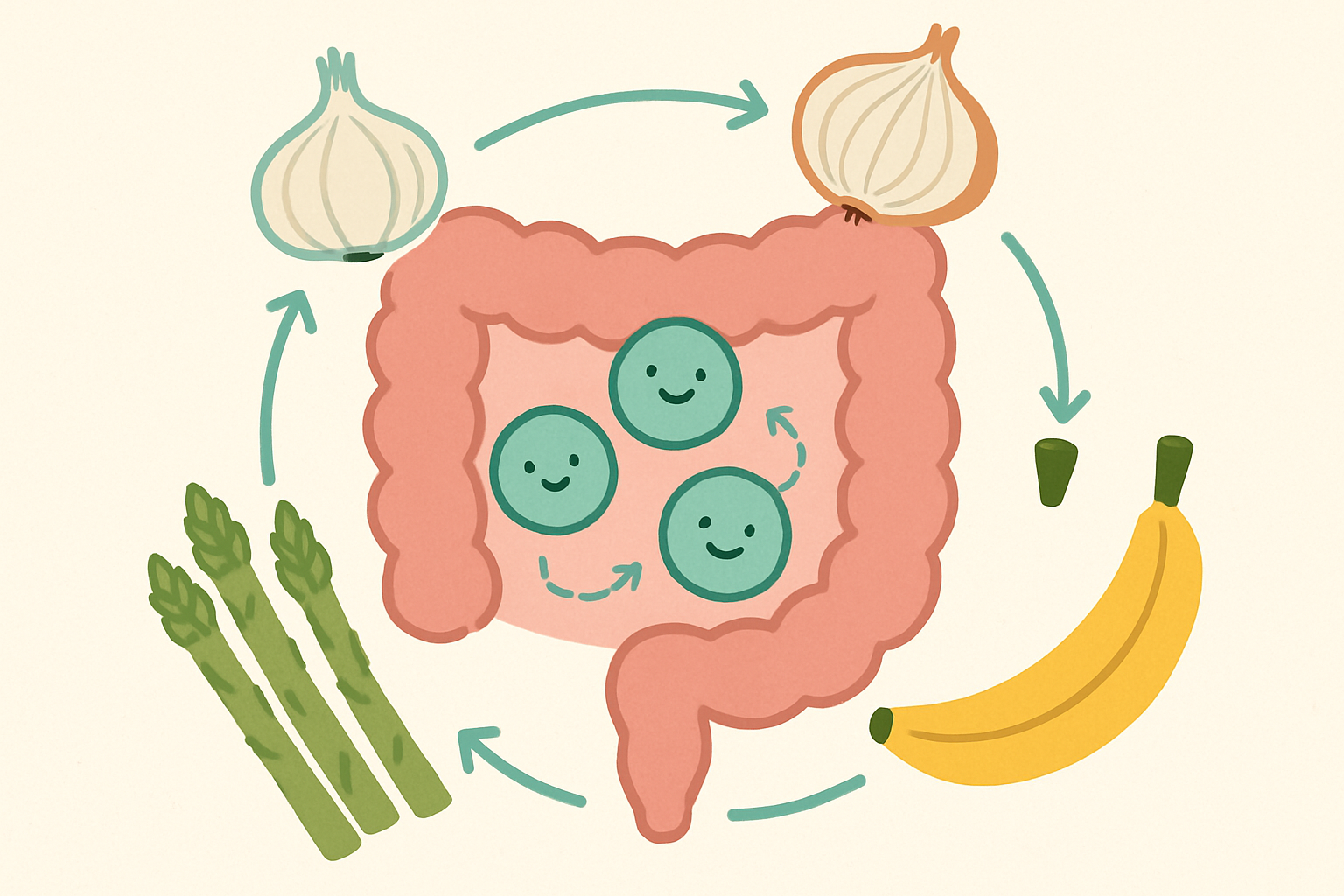
Your top 10 prebiotic foods to add today:
- Garlic (raw or lightly cooked)
- Onions
- Leeks
- Jerusalem artichokes
- Dandelion greens
- Asparagus
- Slightly unripe bananas
- Apples with skin
- Oats
- Flaxseeds
If you’re not used to fiber, start slowly! Begin with one small serving of prebiotic foods daily and drink plenty of water. Gradual introduction prevents the gas, bloating, and discomfort of a sudden fiber increase.
A simple prebiotic-probiotic combo meal: overnight oats made with kefir, topped with sliced banana and a sprinkle of flaxseeds. Or try a lunch bowl with tempeh, sautéed leeks, and asparagus.
Day 6: Anti-Inflammatory Diet Principles
Inflammation can damage your gut lining and disrupt digestion. Today, focus on foods that calm this response.
Include these anti-inflammatory superstars daily:
- Fatty fish like salmon or sardines (omega-3s)
- Extra virgin olive oil
- Walnuts and flaxseeds
- Colorful berries (especially blueberries)
- Leafy greens
- Turmeric (with black pepper to boost absorption)
- Ginger
- Avocados
Balance your plate with roughly 1/2 veggies, 1/4 protein, and 1/4 complex carbs, with a tablespoon or two of healthy fats. This ratio supports gut healing by providing diverse nutrients without overwhelming your digestive system.
Timing matters! Eat your largest meal when you’re most relaxed – usually not during a rushed lunch break. Allow 3-4 hours between meals and avoid eating within 3 hours of bedtime to give your gut a chance to clean and repair overnight.
End your day with gut-healing herbal teas like chamomile, peppermint, or ginger. A potent anti-inflammatory drink: turmeric latte made with warm plant milk, 1/2 teaspoon turmeric, pinch of black pepper, and a touch of honey or cinnamon.
Day 7 and Beyond: Maintaining Your Gut Health Reset
Day 7: Stress Reduction Techniques for Gut Health
Your gut literally has a mind of its own – the enteric nervous system, often called your “second brain.” When you’re stressed, your body releases cortisol and other stress hormones that can throw your digestive system into chaos. This isn’t just theory; it’s why you get butterflies before a big presentation or stomach pain during difficult times.
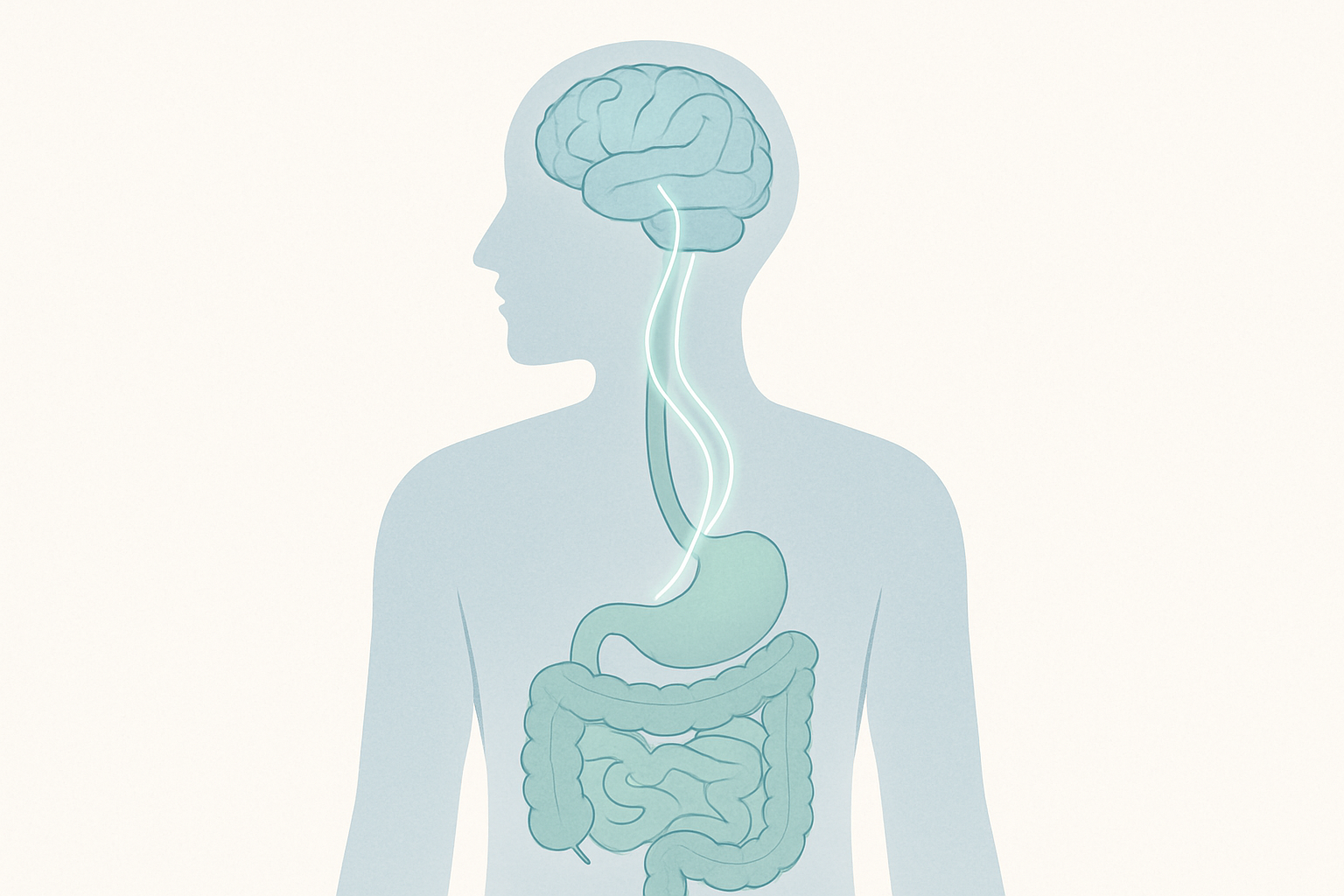
The gut-brain connection works both ways. Reducing stress directly improves your digestion. Here’s how to calm both your mind and your gut:
Quick Belly Breathing: Place one hand on your chest and another on your belly. Breathe deeply for 5 counts, making sure your belly hand rises more than your chest hand. Hold briefly, then exhale for 7 counts. Do this for just 5 minutes when you feel stressed or before meals to switch on your parasympathetic (“rest and digest”) system.
Walk After Meals: A gentle 10-15 minute stroll after eating helps food move through your digestive tract more efficiently. No power walking needed – just a casual pace that allows your body to focus energy on digestion rather than stress response.
Digestive Yoga Poses: Try the “apanasana” (knees-to-chest) pose for 1-2 minutes before bed. Lie on your back, hug your knees to your chest, and gently rock side to side. This massages your intestines and relieves gas. The cat-cow pose also stimulates digestive organs and relieves tension.
Evening Wind-Down: Create a pre-sleep routine that signals to your gut it’s time to rest. Try a warm (not hot) shower, then a cup of chamomile tea. Put away screens at least 30 minutes before bed – blue light disrupts not just sleep hormones but can affect gut hormone production too.
Creating a Sustainable Gut Health Routine
The key to lasting gut health? Balance, not perfection. Follow these practical approaches:
The 80/20 Rule: Aim for gut-friendly choices 80% of the time. The other 20% allows flexibility for special occasions or cravings. This prevents the stress of dietary perfectionism (which ironically damages gut health).
Know Your Personal Triggers: Keep a simple food and symptom journal for two weeks after your reset. Note any foods that consistently cause bloating, pain, or irregular bowel movements. These become your personal “caution foods” – not necessarily banned, but foods to limit.
Meal Prep for Gut Health: Sunday prep of gut-friendly basics saves your digestive system from processed convenience foods. Roast a tray of vegetables, cook a pot of brown rice or quinoa, and prepare some lean protein. Store in glass containers for 2-3 day portions.
Reintroduction Strategy: After your week-long reset, reintroduce potential trigger foods one at a time, waiting 2-3 days between each. Start with small portions (¼ cup) and gradually increase if no symptoms appear. Common culprits to test carefully: gluten, dairy, high-FODMAP foods, and alcohol.
When to Seek Professional Help
While temporary digestive issues are common, certain symptoms warrant medical attention:

Red Flag Symptoms:
- Blood in stool or black, tarry stools
- Unexplained weight loss of 10+ pounds
- Severe abdominal pain, especially if it wakes you at night
- Persistent changes in bowel habits lasting more than 2 weeks
- Difficulty swallowing
Temporary vs. Chronic Issues: Occasional bloating or gas after a rich meal is normal. But symptoms that interfere with daily activities or occur regularly regardless of diet changes suggest underlying issues requiring professional diagnosis.
Helpful Specialists: Start with your primary care doctor, who may refer you to a gastroenterologist (digestive specialist), registered dietitian, or functional medicine practitioner depending on your symptoms.
Key Diagnostic Tests: Your doctor might recommend stool analysis, food sensitivity testing, hydrogen breath tests for SIBO, or comprehensive blood panels to identify problems beyond what diet alone can address.