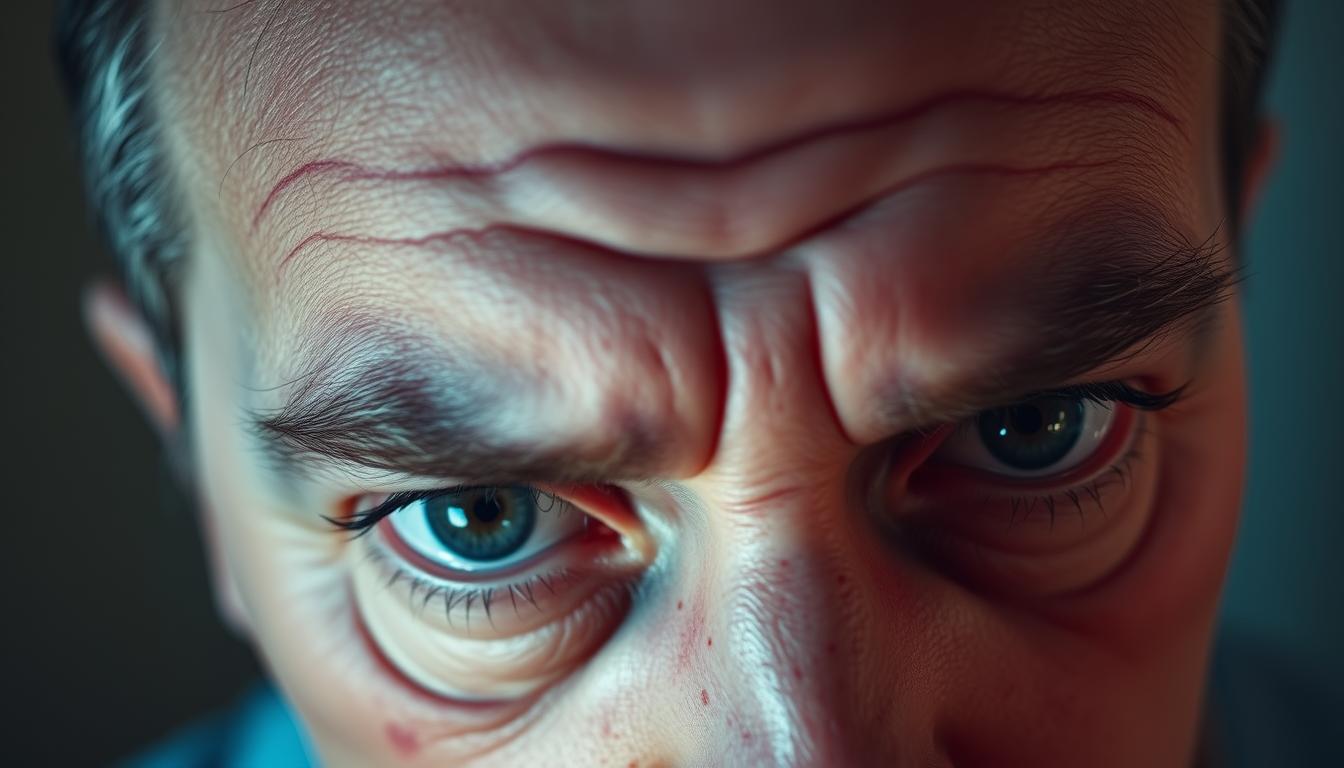
Ever wonder why some people suddenly experience pounding headaches or blurry vision without warning? While hypertension is often called the “silent killer” due to its lack of obvious symptoms, extreme spikes can send unmistakable signals. Let’s explore what happens when your body sounds the alarm.
Most individuals with elevated blood pressure don’t feel different day-to-day. But when readings surge past 180/120 mm Hg, the strain on arteries can create intense pressure in the head. This may trigger throbbing discomfort or visual disturbances as blood flow to critical areas gets disrupted.
Research remains split on whether mild to moderate hypertension directly causes frequent headaches. However, during a hypertensive crisis, the physical effects become undeniable. Recognizing these urgent signs—like sudden vision changes or crushing head pain—could help you act before complications arise.
Key Takeaways
- Most individuals with elevated blood pressure experience no daily symptoms.
- Dangerously high readings (180/120 mm Hg+) may cause severe headaches or vision issues.
- Eye-related changes can include blurred sight or retinal blood vessel damage.
- Ordinary headaches differ from those linked to extreme blood pressure spikes.
- Prompt medical care is crucial during hypertensive emergencies.
The Connection Between High Blood Pressure and Headaches
Have you ever had a headache that felt different from your usual tension-type pain? Many people don’t realize that extreme cardiovascular strain might create distinct sensations in the head. While most individuals with elevated readings experience no daily effects, sudden spikes can trigger unmistakable physical signals.

Identifying Common Symptoms
When discomfort does occur, it often appears as rhythmic pulsing on both sides of the head. The Iranian Journal of Neurology notes this bilateral pattern frequently intensifies during exercise or movement. Physical exertion may worsen the throbbing sensation as strained blood vessels struggle to manage increased circulation demands.
The American Heart Association clarifies that these symptoms typically emerge only when readings surpass 180/120 mm Hg. At this critical level, fluid leakage through compromised blood-brain barriers can lead to swelling. This pressure buildup creates pain distinct from ordinary tension headaches.
Reviewing Research Findings
Studies present conflicting conclusions about routine discomfort in those with elevated cardiovascular measurements. A 30-year study tracking 1,914 participants found no increased heart risks for those experiencing frequent head pain. However, hypertensive crises remain undisputed triggers for severe episodes requiring urgent care.
Medical professionals emphasize that persistent discomfort alongside elevated readings warrants evaluation. As one researcher states: “While daily headaches might not predict complications, sudden severe pain with visual changes demands immediate attention.” This distinction helps people recognize when to seek help versus when to monitor patterns.
How High Blood Pressure Makes Your Head and Eyes Feel
Imagine feeling like your head is trapped in a tightening vise while the world around you blurs unexpectedly. Extreme cardiovascular strain can trigger this alarming combination of physical sensations. When arteries endure excessive force, fluid may leak into brain tissue, causing swelling that presses against the unyielding skull.

This pressure buildup often manifests as a dull, persistent ache rather than sharp pain. Blood vessel walls in the brain stretch beyond their limits, creating throbbing discomfort that worsens with movement. Unlike tension headaches, this pain typically affects both sides of the head simultaneously.
Visual disturbances frequently accompany these episodes. Retinal arteries may narrow or develop tiny tears, causing sudden blurred vision or floating spots. Some people report temporary “blind spots” or light flashes – clear indicators of ocular strain from elevated readings.
Neurological effects compound the physical discomfort. Swelling in the brain can lead to dizziness, confusion, or difficulty focusing. These symptoms create a disorienting experience where simple tasks feel overwhelming. As one cardiologist notes: “When patients describe head pressure with visual changes, we treat it as a potential emergency.”
Recognizing these warning signs proves crucial. A crushing sensation paired with sight alterations often signals readings above 180/120 mm Hg. Immediate medical evaluation helps prevent lasting damage to delicate neural and ocular tissues.
Underlying Causes and Risk Factors
What really drives those silent changes in your cardiovascular system? While many assume hypertension strikes randomly, it often stems from a mix of invisible triggers and daily habits. Let’s unpack why some people face higher risks and how these elements interact over time.
Lifestyle and Genetic Influences
Your DNA plays a bigger role than you might think. If close relatives have cardiovascular issues, your chances of similar challenges rise significantly. But genes aren’t destiny – daily choices amplify or soften their impact.
A salty diet, frequent alcohol use, and couch-bound routines quietly strain arteries. Smoking tightens blood vessels like a clenched fist, while chronic stress floods your system with tension hormones. These factors team up to push numbers upward, often before noticeable symptoms appear.
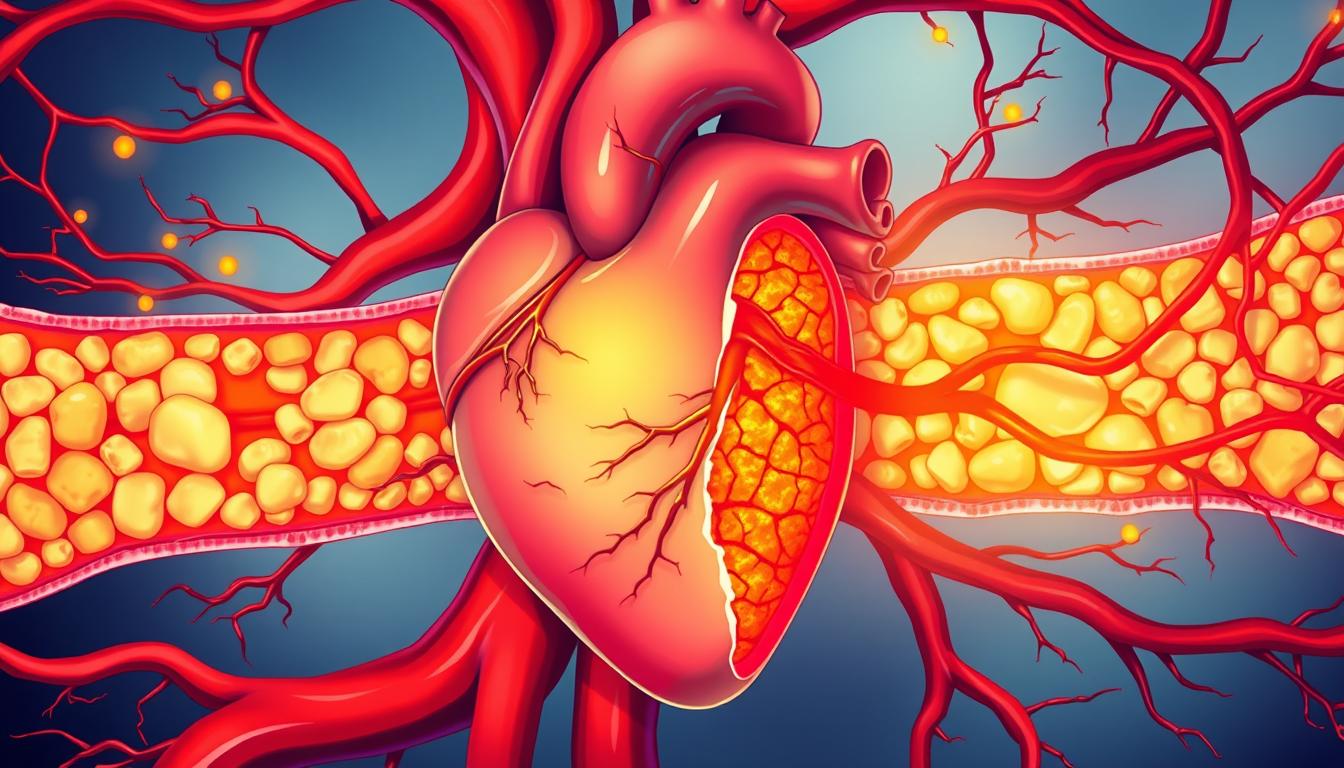
Impact on Vital Organs
Unchecked hypertension acts like slow-acting poison for critical systems. Your heart muscle thickens from constant overwork, reducing its efficiency. Kidneys struggle to filter waste as their tiny blood vessels stiffen, potentially leading to irreversible damage.
| Organ | Effects | Contributing Factors |
|---|---|---|
| Heart | Thickened muscle, heart failure risk | Chronic strain, obesity |
| Kidneys | Reduced filtration, protein leakage | Damaged vessels, diabetes |
| Brain | Memory issues, stroke potential | Narrowed arteries, aging |
The brain suffers too – reduced blood flow can cloud thinking and increase dementia risks. As one nephrologist notes: “Controlling cardiovascular health protects multiple systems at once. It’s like fixing a leaky roof before the storm hits.”
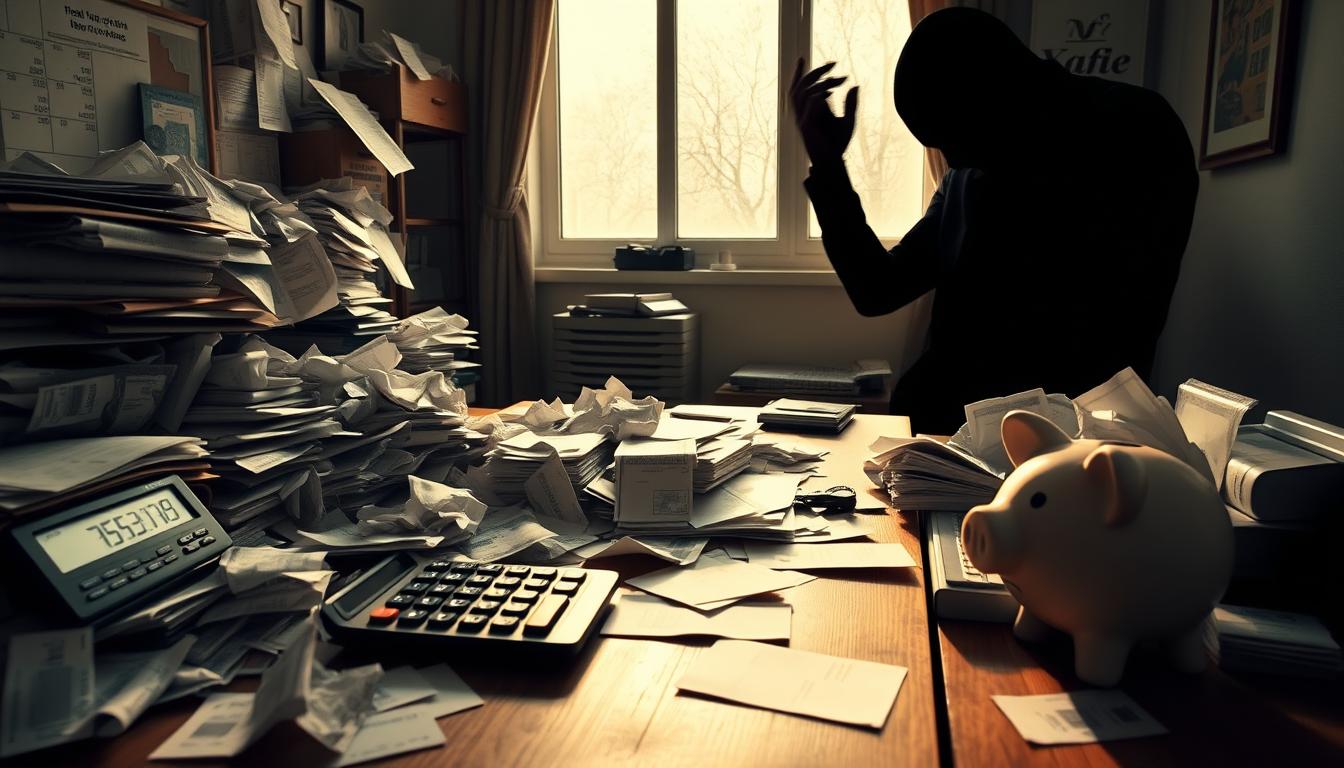
Recognizing Emergency Scenarios
When your body sends distress signals, knowing how to respond can be life-saving. Readings above 180/120 mm Hg demand immediate attention – but not all spikes behave the same way. Understanding the difference between urgent and critical situations helps you act appropriately when minutes matter.
Distinguishing Hypertensive Crisis from Urgency
Hypertensive urgency involves severely elevated numbers without immediate organ damage. You might feel anxious but still manage basic tasks. In contrast, a full-blown crisis brings physical changes like chest tightness or slurred speech – signs your body’s systems are failing.
Emergency rooms use this key distinction: urgency requires monitoring and gradual reduction, while crisis needs rapid treatment to prevent stroke or heart damage. As one ER nurse explains: “We’re not just lowering numbers – we’re protecting brains and kidneys from shutting down.”
When to Seek Immediate Medical Help
Dial 911 if you experience any of these alongside high readings:
- Crushing chest pain spreading to your arm
- Sudden vision loss or double images
- Inability to move one side of your body
Emergency teams use IV medications like labetalol to safely reduce cardiovascular strain. Trying to self-treat with extra pills could dangerously disrupt blood flow to vital organs. Remember – urgent care clinics can’t manage these crises. Only hospitals have the monitoring equipment and specialists needed.
Studies show 4.6% of patients in coronary units don’t survive hypertensive emergencies. Quick action significantly improves outcomes. Keep emergency contacts visible, and don’t hesitate to seek help – it’s always better to err on the side of caution.
Managing and Treating High Blood Pressure
Taking charge of your cardiovascular health requires both smart strategies and daily commitment. While medications play a vital role, lasting improvement often comes from combining prescription solutions with personalized lifestyle changes.
Medication Options and Lifestyle Adjustments
Doctors often prescribe ACE inhibitors or calcium channel blockers to relax blood vessels. These treatments work best when paired with consistent exercise and sodium reduction. “The right combination differs for everyone,” notes cardiologist Dr. Elena Torres. “A marathon runner might need different care than someone managing diabetes.”
Small daily changes create big impacts. Losing just 5-10 pounds can improve readings. Brisk walking strengthens heart muscles better than sporadic gym visits. Stress-reduction practices like box breathing help prevent sudden spikes.
Over-the-Counter Remedies and Dietary Tips
For occasional head discomfort, acetaminophen remains safer than NSAIDs for those on blood pressure medications. Track food triggers using phone apps – aged cheeses and cured meats cause issues for 20% of people.
Try these kitchen swaps:
- Use smoked paprika instead of bacon bits
- Choose fresh herbs over salty seasonings
- Opt for dark chocolate instead of processed sweets
Home monitoring kits provide real-time feedback between doctor visits. Pair measurements with mood notes to spot stress-related patterns. Remember – managing this condition isn’t a sprint, but a lifelong journey toward better health.
Conclusion
Staying alert to your body’s signals could be the difference between temporary discomfort and lasting damage. While hypertension often develops quietly, extreme spikes create unmistakable warnings like crushing head pain or sudden vision shifts.
Regular check-ups become your first defense against silent threats. Most people with elevated readings won’t feel daily effects, but those 180/120 mm Hg+ moments demand swift action. Pair home monitoring with honest conversations about symptoms during medical visits.
Effective management combines smart habits with professional guidance. Simple swaps like walking after meals or using herbs instead of salt add up over time. Treatment plans work best when tailored to your unique health profile and lifestyle needs.
Remember – head discomfort with skyrocketing numbers isn’t normal. Other conditions can mimic these signs, so proper evaluation matters. Build trust with your care team to navigate both prevention strategies and urgent situations confidently.
Your cardiovascular health thrives on consistency. Small daily choices protect your head, eyes, and vital organs better than any emergency intervention. Stay curious, stay proactive, and let knowledge power your prevention journey.