The Strange Connection Between Your Gut and Your Mood

Photo by Alisha Mishra on <a href="https://www.pexels.com/photo/clear-glass-bottle-filled-with-broccoli-shake-1346347/" rel="nofollow">Pexels.com</a>
The Science Behind Your Gut Microbiome and Mental Health
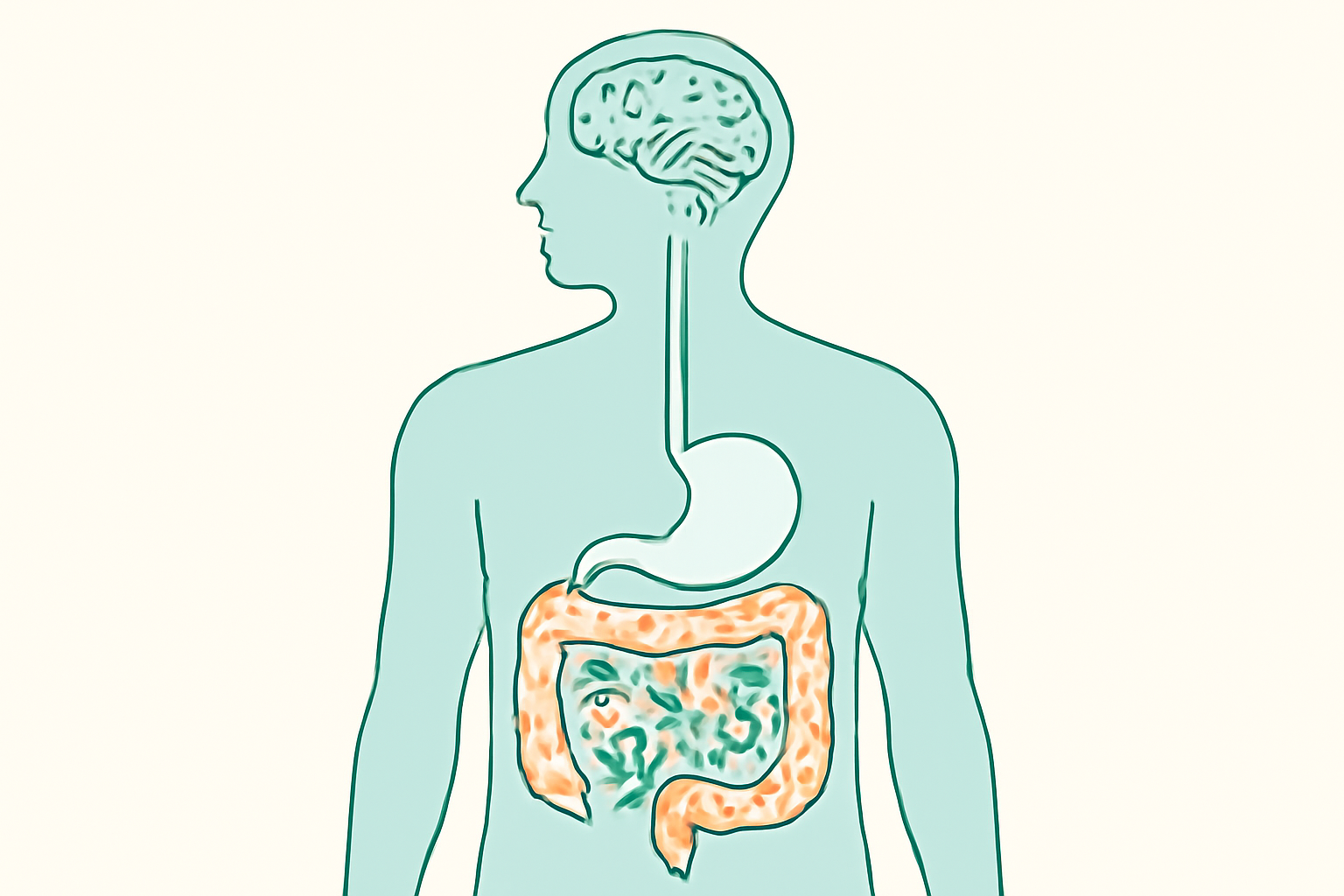
Meet Your Second Brain: The Enteric Nervous System
Have you ever felt butterflies in your stomach before a big presentation? Or experienced gut pain during times of stress? This isn’t coincidence—it’s your enteric nervous system (ENS) at work.
Your gut houses an incredible network of over 100 million neurons—more than found in your entire spinal cord. This complex system forms what scientists call your “second brain,” and it’s revolutionizing how we understand mental health.
The ENS operates independently from your brain, controlling digestive functions without needing constant input from upstairs. But what makes this system truly remarkable is its two-way communication with your brain through the vagus nerve. This constant back-and-forth dialogue explains why digestive issues often accompany anxiety and depression.
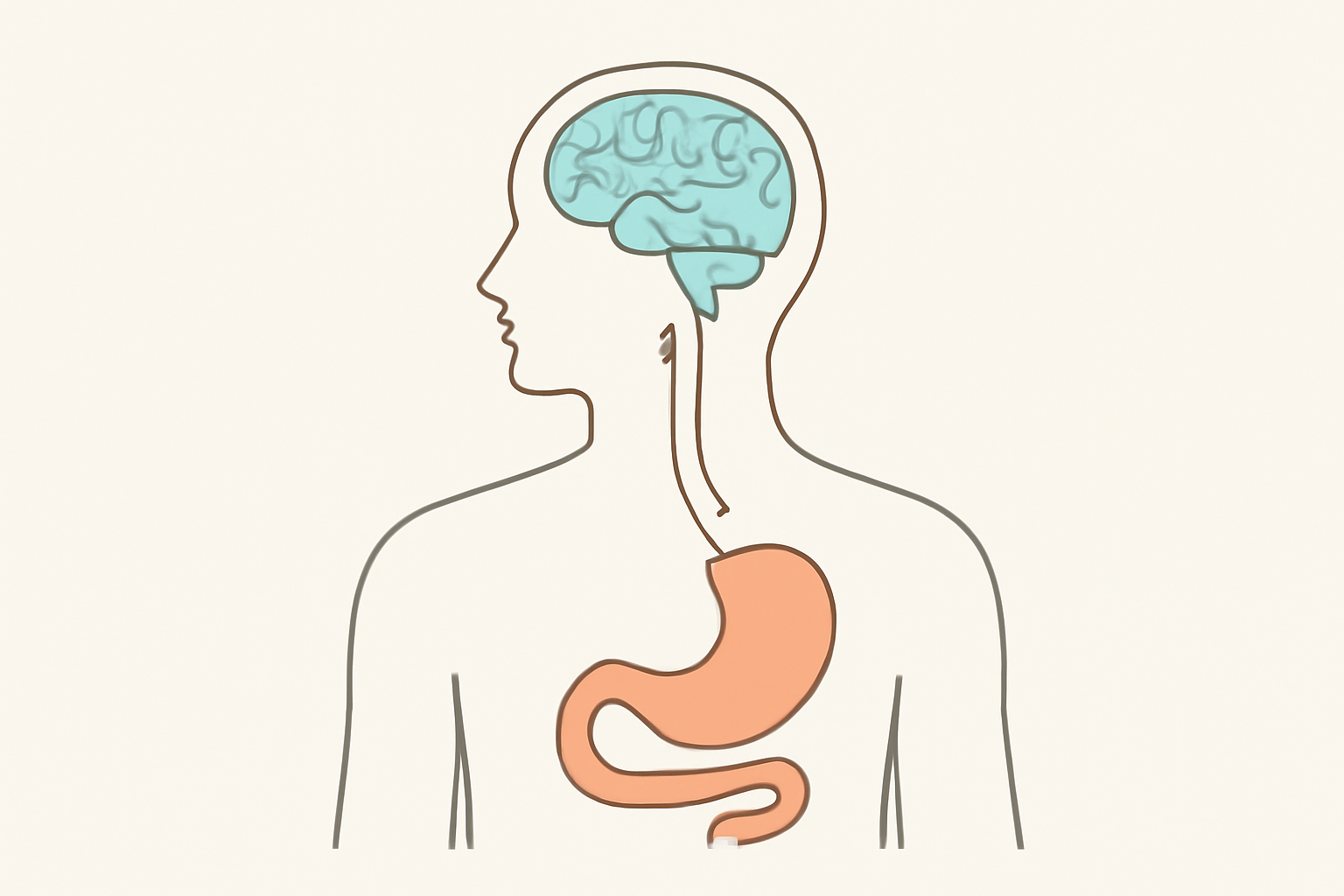
Perhaps most surprising is that up to 90% of your body’s serotonin—the “happy chemical” targeted by many antidepressants—is actually produced in your gut, not your brain. This fact alone has transformed our understanding of mood disorders, suggesting that proper gut health might be as important as brain health for emotional wellbeing.
How Your Gut Microbiome Influences Neurotransmitter Production
The trillions of bacteria in your gut microbiome don’t just help digest food—they’re active participants in your mental health. These microscopic residents directly produce and influence key neurotransmitters that regulate your emotions.
Your gut bacteria manufacture important mood-regulating chemicals including GABA (which calms anxiety), dopamine (involved in pleasure and motivation), and serotonin (which regulates happiness and satisfaction).
 When your gut microbiome falls out of balance, these neurotransmitter systems can falter, potentially triggering mood disturbances.
When your gut microbiome falls out of balance, these neurotransmitter systems can falter, potentially triggering mood disturbances.
Research has identified specific bacterial heroes in this process. Certain strains of Lactobacillus and Bifidobacterium have been directly linked to increased production of GABA, which helps explain why probiotics containing these bacteria sometimes reduce anxiety symptoms in both animal and human studies.
🔥 If you want better energy, better gut health, and better results, you can’t wait.
Grab your LoveBiome essentials now
The Vagus Nerve: Your Gut-Brain Information Highway
The vagus nerve serves as the primary communication channel in your gut-brain axis—a sophisticated information superhighway carrying signals in both directions.
When your gut microbiome is healthy, positive signals travel up to your brain, supporting emotional regulation. But when gut health suffers, inflammatory signals can travel this same pathway to disrupt brain function, potentially triggering anxiety, depression, and even cognitive changes.
Interestingly, you can actively strengthen this connection through vagus nerve stimulation. Simple practices like deep breathing, gargling, cold water face immersion, and even humming can stimulate the vagus nerve, improving both digestive function and mood regulation simultaneously.
Inflammation: The Common Denominator in Gut and Mental Health Issues
Emerging research points to inflammation as the critical link between gut health and mental wellbeing. When your intestinal barrier becomes compromised (often called “leaky gut”), inflammatory compounds can escape into your bloodstream and eventually reach your brain.
This systemic inflammation has been strongly associated with depression, anxiety disorders, and other mood disturbances. In fact, many researchers now view depression partially as an inflammatory condition, explaining why anti-inflammatory approaches sometimes improve mood symptoms.
The good news? Certain gut bacteria species act as natural anti-inflammatory agents. By nurturing these beneficial microbes through diet and lifestyle changes, you can potentially reduce systemic inflammation and improve both gut health and mood simultaneously.
Practical Ways to Optimize Your Gut Microbiome for Better Mental Health
Dietary Changes That Support Both Gut and Brain Health
Your gut microbiome—the trillions of bacteria living in your digestive tract—plays a crucial role in your mental wellbeing.
 Fortunately, you can actively nurture these beneficial microbes through strategic dietary choices.
Fortunately, you can actively nurture these beneficial microbes through strategic dietary choices.
🚨 Every day you delay is another day you feel less than your best. Take action fast.
Start your LoveBiome journey immediately
Start by incorporating prebiotic-rich foods into your daily meals. Prebiotics are special plant fibers that your body can’t digest but that feed your beneficial gut bacteria. Excellent sources include garlic, onions, leeks, asparagus, bananas, and Jerusalem artichokes. These foods contain inulin and fructooligosaccharides (FOS) that specifically nourish Bifidobacteria and Lactobacilli—bacterial strains linked to reduced anxiety and depression symptoms. Try adding raw garlic to salad dressings or roasting Jerusalem artichokes as a side dish.
Fermented foods deliver a double benefit by introducing live beneficial bacteria directly into your gut ecosystem. Yogurt with live cultures, kefir, kimchi, sauerkraut, and kombucha are all excellent options. Even a small daily serving—just a few tablespoons of sauerkraut or a cup of kefir—can significantly impact your gut health over time. Research shows that regular consumption of these foods correlates with improved mood regulation and reduced anxiety symptoms.
The Mediterranean diet pattern offers perhaps the most comprehensive approach to gut-brain health. This eating style emphasizes:
- Colorful fruits and vegetables rich in polyphenols
- Olive oil and nuts containing anti-inflammatory omega-3 fatty acids
- Whole grains providing diverse fibers for microbiome diversity
- Fish and moderate amounts of poultry
Just as important as what to include is what to minimize. Processed foods, artificial sweeteners, and excessive alcohol all disrupt the delicate balance of your gut microbiome. Many ultra-processed foods contain emulsifiers that can damage the protective mucus layer in your intestines, potentially contributing to inflammation that affects your brain.
Targeted Probiotic Strategies for Mental Wellbeing
While dietary changes form your foundation, specific probiotic supplements can provide additional support for your mental health. Not all probiotics are created equal when it comes to mood regulation.
Three strains have shown particular promise: Lactobacillus acidophilus, Bifidobacterium longum, and Lactobacillus rhamnosus. These bacteria influence neurotransmitter production and can reduce stress hormones like cortisol. Clinical studies demonstrate that participants taking these strains experience measurable reductions in anxiety and depression scores compared to placebo groups.
When selecting a probiotic supplement, look for multi-strain formulas. Different bacterial species perform complementary functions in your gut, creating a synergistic effect that single-strain supplements can’t match. The timing and consistency of your probiotic routine matter more than extremely high doses—taking a moderate-dose probiotic consistently with meals provides better results than sporadic high-dose supplementation.
Lifestyle Factors That Influence Your Gut Microbiome and Mood
Your gut health doesn’t exist in isolation from the rest of your life.
 Physical activity profoundly affects both your microbiome diversity and mental wellbeing. Even modest exercise—a 20-minute walk several times weekly—stimulates gut motility, reduces inflammation, and boosts mood-regulating neurotransmitters.
Physical activity profoundly affects both your microbiome diversity and mental wellbeing. Even modest exercise—a 20-minute walk several times weekly—stimulates gut motility, reduces inflammation, and boosts mood-regulating neurotransmitters.
Stress management deserves special attention in any gut-brain health plan. Chronic stress alters gut permeability and bacterial composition, creating a vicious cycle of inflammation and mood disturbance. Mindfulness meditation, deep breathing exercises, and progressive muscle relaxation all directly benefit both gut function and mental state. Just 10 minutes of meditation daily can make a measurable difference in both digestive symptoms and anxiety levels.
Quality sleep represents another pillar of gut-brain health. Your gut microbiome follows a circadian rhythm, and disrupted sleep patterns can rapidly alter the microbial balance. Prioritize 7-9 hours of sleep in a dark, cool room, and consider establishing a consistent bedtime routine. Scientists have discovered that even short-term sleep disturbance reduces beneficial bacterial strains and increases inflammatory markers.
Don’t underestimate the power of nature exposure. Gardens, forests, and natural environments introduce beneficial environmental microbes that may improve mental resilience. Walking barefoot in natural settings or gardening without gloves provides direct contact with diverse microbial communities that can enhance your own gut ecosystem.
When to Seek Professional Help for Gut-Brain Issues
While self-directed dietary and lifestyle changes benefit most people, persistent digestive issues accompanied by anxiety or depression warrant professional consultation. Pay attention to warning signs like chronic bloating, irregular bowel movements, and unexplained mood changes that don’t respond to basic interventions.
Several types of healthcare providers specialize in the gut-brain connection. Functional medicine practitioners take a systems-based approach to identify underlying causes of both digestive and mental health symptoms. Gastroenterologists can rule out serious digestive conditions, while nutritional psychiatrists specialize in food-mood connections.
Consider advanced testing options like comprehensive stool analysis to assess your microbiome composition, organic acid testing to evaluate bacterial metabolites, and food sensitivity testing to identify potential inflammatory triggers. These tests provide personalized data that can guide your treatment plan beyond general recommendations. The American Psychiatric Association recognizes that gastrointestinal symptoms frequently accompany depression and anxiety, making integrated care increasingly important.
⚡ Your health isn’t going to fix itself. Start fueling your body the right way—right now.
Transform your wellness today